Which Of The Following Is The Primary Reason For The Growth In Outpatient Services?
Medical procedures are moving into outpatient facilities, mainly due to technological advances such as minimally invasive surgical procedures. But value-based care incentives are also playing a part in this tendency.
Executive summary
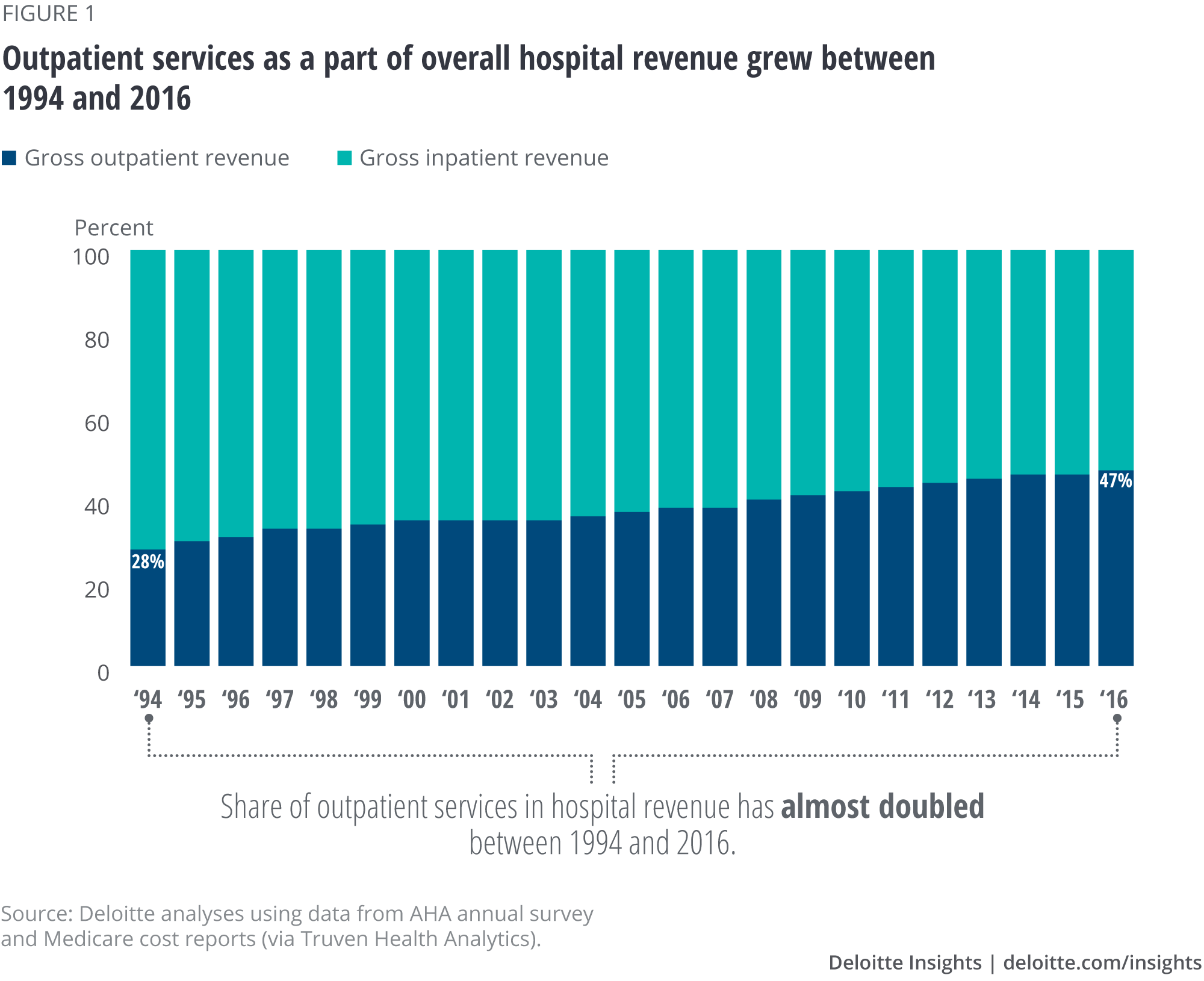
Clinical innovation, patient preferences, and fiscal incentives are tilting the residue in favor of outpatient settings for hospital services. Aggregate hospital acquirement from outpatient services grew from xxx percentage in 1995 to 47 percent in 2016.1 Some of this alter is driven by patient preference and clinical and technological advances such every bit minimally invasive surgical procedures and new anesthesia techniques that reduce complications and let patients to return home sooner.
Financial incentives have likely played a role besides. Wellness plans and regime programme payment policies back up providing services in lower-cost care settings, including outpatient facilities.2 Health systems have too been acquiring or partnering with physicians and dr. practices, farther driving up the book of services3 performed in outpatient settings.four
Moreover, these payers also are often using shared-savings, bundles, and other arrangements that necktie payment amounts to cost and quality performance. One reason for the growth in outpatient care might be health systems' strategies to perform well under these arrangements past reducing inpatient care past shifting patients to outpatient settings. To proceeds greater insight into the factors driving growth in outpatient services and reject in inpatient care, the Deloitte Center for Health Solutions conducted descriptive and regression analyses using Medicare claims data between 2012 and 2015. Three fundamental findings emerged:
- Hospitals with greater revenues from quality and value contracts provided more outpatient services than other hospitals. Hospitals that derive a large part of their revenue from quality and value contracts had 21 percent more Medicare outpatient visits and xiii percent higher outpatient revenue between 2012 and 2015 (even after controlling for hospital characteristics), compared with hospitals that did non report acquirement from such contracts.
- The clan betwixt having these contracts and higher outpatient services was even more pronounced for sure therapeutic areas. The relationship was strongest for major diagnostic categories (MDCs) with higher rates of physician-infirmary affiliation and technological change. Outpatient acquirement was eighteen per centum higher for diseases of the circulatory organization5 and 13 percent college for diseases of the musculoskeletal organisationhalf-dozen among hospitals with big incentives.
- All hospitals saw declines in inpatient revenues, but hospitals with greater revenues from quality and value contracts did non see steeper declines than other hospitals. The lack of a relationship between quality and value contracts and inpatient intendance may be because wellness systems are not yet at sufficient risk to actively manage population wellness to reduce inpatient care more aggressively.
Given the shift from inpatient to outpatient care, health systems will want to consider building effective strategies to grow capacity and infrastructure for outpatient services. These strategies mostly have three components:
- Human and concrete capital letter. Expanding outpatient services may telephone call for additional physical and man capital (or their re-configuration) and workflow and operational improvements. Building physician relationships and networks through partnerships or affiliations (including with nontraditional wellness care entities such as retail health clinics) can assist build chapters and concenter patients.
- Virtual care/technology. Investing in virtual intendance/engineering capabilities could expand outpatient services while too helping hospitals bend the cost curve and heave revenue.
- Case management/analytics. Health systems tin work with physicians to utilize analytics and with patients to decide on which care setting is the nearly effective, rubber, and efficient.
Infirmary outpatient care is growing
Hospital inpatient stays take declined 6.6 percentage over the by decade despite population growth and demographic shifts (such as an increasingly older, sicker Medicare population).vii In contrast, between 2005 and 2015, visits to outpatient facilities (run into sidebar "Blazon of outpatient care settings") increased by 14 percent—from 197 visits per 100 people in 2005 to 225 visits per 100 people in 2015.eight Hospitals' gross outpatient revenue per visit increased at an even faster pace. Between 2010 and 2015, gross outpatient revenue per visit grew 45 percent, from $1,352 per visit in 2010 to $ane,962 per visit in 2015.9 Health systems and hospitals have also increased their capital investments in outpatient facilities.10 As a outcome, as effigy one illustrates, the amass share of outpatient services in total hospital acquirement has grown over time—from 28 percentage in 1994 to almost half (47 percent) in 2016.
Types of outpatient care settings
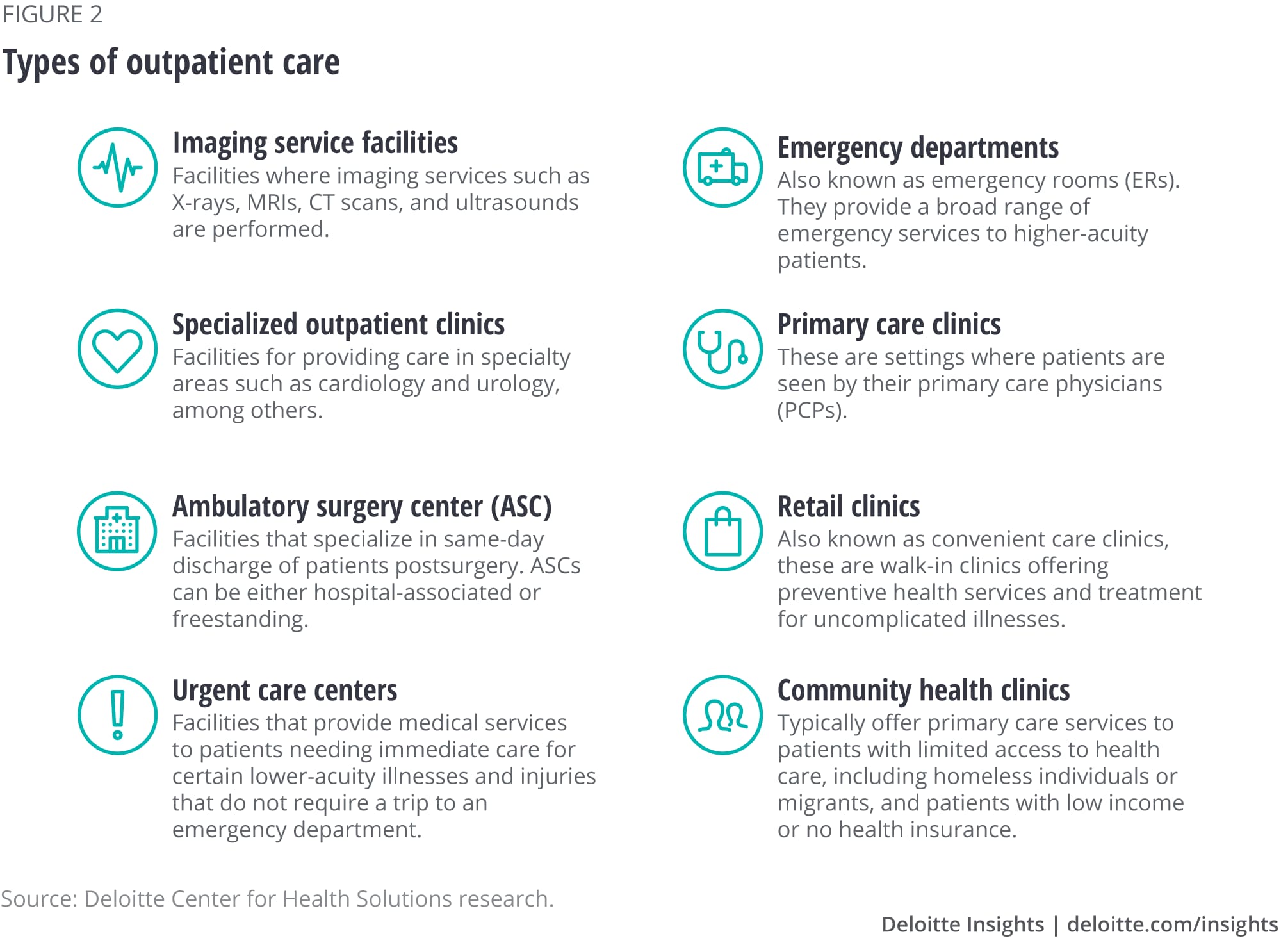
Wellness care services can exist categorized into inpatient and outpatient depending on where the procedure is performed and the length of stay. Outpatient care refers to medical services and procedures, typically low-acuity ones that exercise not require an overnight hospital stay. Figure 2 beneath describes the chief types of hospital-based outpatient facilities.
Variation in outpatient services across states
Between 2012 and 2015, outpatient revenue grew faster than inpatient revenue in all but two states, according to our analyses. Only, as figure 3 shows, the mix of infirmary inpatient and outpatient services in 2015 varied significantly past state. In Nevada, for example, outpatient services accounted for 35 percent of full hospital revenue, while they fabricated up 69 percent of Vermont hospitals' revenue. This variation largely reflects a combination of regional differences in physician practice patterns and other market factors.

The increase in infirmary outpatient services was pronounced in Medicare fee for service (FFS) between 2005 and 2015. During this period, outpatient services per casher—which include outpatient visits and imaging services—grew 47 percentage, according to the Medicare Payment Advisory Commission (MedPAC). Between 2006 and 2015, Medicare outpatient spending per beneficiary grew 8 percent annually from $885 in 2006 to $1,753 in 2015, according to MedPAC.xi
What is driving the shift of hospital services to outpatient settings?
Innovation and improvements in clinical procedures probable played an of import role in enabling this change.12 Many surgeries and medical and diagnostic procedures that once required an inpatient stay tin now be performed safely in an outpatient setting. Patients have embraced these changes every bit outpatient services tend to cost less—and be more convenient—than inpatient services. Inpatient facilities tend to maintain more staff and have a wider range of capabilities, services, and equipment, including resources-intensive technologies that drive up costs. Furthermore, minimally invasive surgical procedures—such every bit laparoscopy and robotic surgery—and new anesthesia techniques that help prevent complications, take helped reduce recovery time for outpatient services and improved patient convenience.
Under Medicare payment policy, on-campus hospital-owned physician practices are paid more than independent physicians for the same services, which provides health systems with the incentive to buy physician practices.13 A MedPAC written report institute that physician-hospital consolidation increased between 2012 and 201414 and that in 2014, 39 percent of physicians who billed for Medicare in a large national database were affiliated with a health arrangement or hospital. This consolidation could lead to more services being performed in infirmary outpatient settings.
In add-on to these trends, the increase in value-based payments might spur greater shifts from inpatient to outpatient care, to reduce full cost of care and amend patient experience. Health plans and Medicare and Medicaid programs are experimenting with payment models that reward better value (come across sidebar "Main types of quality and value contracts"). These provide participating health systems with the incentive to shift services to lower-cost care settings, including outpatient ones.15 Indeed, some wellness care systems are building clinically integrated networks to help them perform more effectively in quality and value-payment models, partly by acquiring or partnering with physicians and medico practices.16
We wanted to explore whether hospitals that receive a higher share of revenue from quality and value contracts are seeing more services shift to outpatient settings. This question has not been studied well then far. We analyzed inpatient and outpatient claims data from a nationally representative v percent sample of Medicare beneficiaries from 2012 to 2015. We combined this data with data most hospital and market characteristics—such as hospital size, location (urban or rural), ownership type, teaching status, and case and payer mix. We also categorized hospitals by the degree to which they receive revenue from quality and value contracts (encounter the Appendix for further details).
Principal types of quality and value contracts
Some health plans are tying payment to provider toll and quality performance through new payment arrangements such every bit:
- Shared savings. Under this system, a provider system is typically paid on a fee-for-service footing, simply full annual spending is compared with a target. If spending is beneath that target, the organization receives a per centum of the savings (relative to the target) as a bonus.
- Shared risk. In addition to sharing savings (relative to a target), if a provider organization spends more than than the target corporeality, it must repay some of the difference as a punishment.
- Bundled payments. Instead of paying separately for the infirmary, physician, and other services, a wellness plan bundles payment for all services linked to a status, reason for the hospital stay, and period of treatment. An organization tin can proceed the money it saves through reduced spending on some component(s) of intendance included in the packet.
- Partial/global capitation payments. An organization receives a per-person payment (usually per-month) intended to pay for all, or a specified subset, of individuals' intendance, regardless of the services used.
Hospitals with higher quality and value incentives accept more outpatient visits and revenue
We used hospital revenue information from quality and value contracts ("incentives") to allocate hospitals into iii groups (run across the Appendix for details):
- Hospitals with large (in a higher place the median) incentives;
- Hospitals with pocket-sized (below the median) incentives; and
- Hospitals that report receiving no revenue from quality and value contracts.
Between 2012 and 2015, hospitals with whatever acquirement from quality and value contracts accounted for about 10 percent of the approximately iii,500 hospitals in our database. We divided that group into 2: those with big incentives had an average of 23 percent of their revenue from quality and value contracts, and those with small incentives received iii percentage of their revenue from such arrangements.
Hospitals with whatever incentives (large or small-scale) mostly differed from the remainder. Hospitals with large incentives were more likely to be medium-sized (48 percent vs. 34 pct) and not for profit (73 percent vs. 49 percent), as well as to take a asymmetric share condition (68 percent vs. 44 pct) and college patient instance mix (i.14 vs. 0.7), compared to hospitals with no incentives. To control for the possible influence of infirmary characteristics on the association between outpatient services mix and quality and value incentives, we used a seemingly unrelated regressions estimation framework (encounter the Appendix).
Regression results reveal that, on boilerplate and decision-making for their other characteristics, hospitals with any incentives had more outpatient visits and revenue than other hospitals. Moreover, nosotros saw an even stronger human relationship betwixt outpatient services and quality and value contracts for hospitals with large incentives (figure 4). Compared with hospitals that did not report whatsoever revenue from quality and value contracts:
- Hospitals with large incentives had 21 percent more outpatient visits and 13 percent more outpatient acquirement.
- Hospitals with small-scale incentives had xvi percent more outpatient visits.
Even so, we did not see larger drops in inpatient visits and revenue for hospitals with any incentives, compared with other hospitals during the period nosotros examined (figure 4).

Therapeutic areas with largest rates of physician-hospital affiliation and technological change saw the largest increases
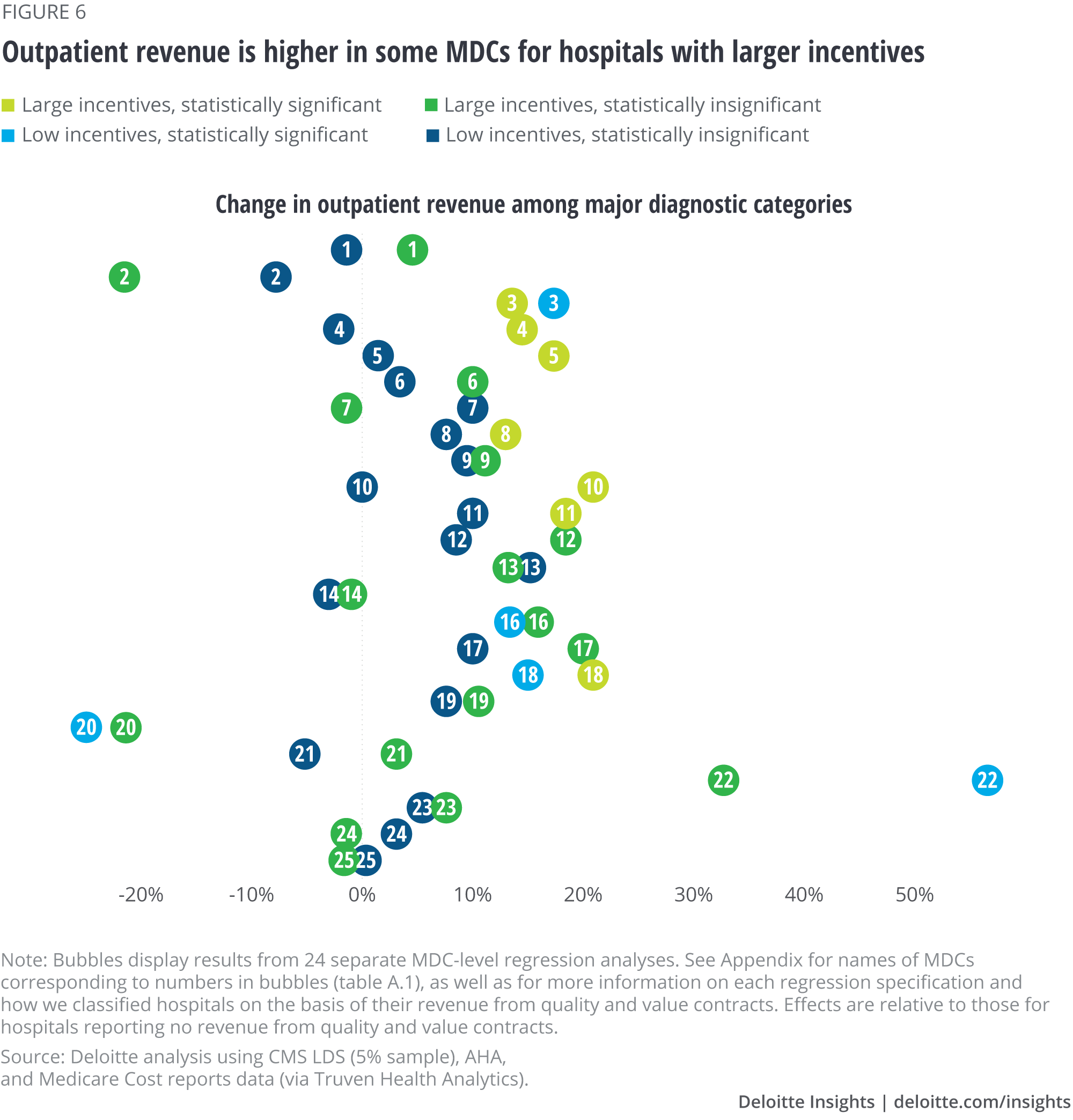
Was the relationship between growth in outpatient services and presence of incentives more than pronounced in sure therapeutic areas? We found the relationship was strongest for major diagnostic categories (MDCs) with higher rates of physician-infirmary affiliation and technological modify. Outpatient revenue was xviii percent college for diseases of the circulatory organisation17 and xiii percent higher for diseases of the musculoskeletal organization18 among hospitals with large incentives.
Nosotros institute that compared to hospitals reporting no revenue from quality and value contracts:
- Hospitals with big incentives had more outpatient visits than those with no incentives for xiv of the 24 MDCs that we studied (figure five; for more details on MDCs, see the Appendix). We generally saw a stronger association for hospitals with big incentives. For example, outpatient visits for endocrine and metabolic diseases and disorders were 37 percent higher amongst hospitals with large incentives (MDC 10 in effigy 5) than amongst hospitals with no incentives. Outpatient visits for diseases and disorders of the kidneys, blood, male person reproductive system, and mental wellness diseases were 20–22 per centum college amongst hospitals with the largest incentives (MDCs 11, 12, 16 and 19 in figure 5).
- Hospitals with large incentives had higher outpatient revenue than those with no incentives for 7 of the 24 MDCs that we studied: diseases and disorders of the ear, olfactory organ, and mouth (MDC iii in figure 6); respiratory system (MDC 4); circulatory system (MDC 5); musculoskeletal system (MDC eight); endocrine, nutritional, and metabolic system (MDC x); kidney and urinary tract (MDC 11); and infectious and parasitic diseases (MDC 18).
- We did not meet statistically significant reductions in inpatient visits and revenue amid hospitals with quality and value incentives for whatever of the MDCs that we studied. There are three possible reasons for this finding—one, information technology may exist that in that location are too few hospitals with major exposure to contracts to find an consequence. Two, information technology may be that hospitals are early on into their population health strategies and starting with building outpatient chapters rather than decreasing inpatient care aggressively (especially given that they are still paid under fee-for-service for a significant share of their business). Finally, our information may not capture the nuances of the take a chance borne under these contracts.
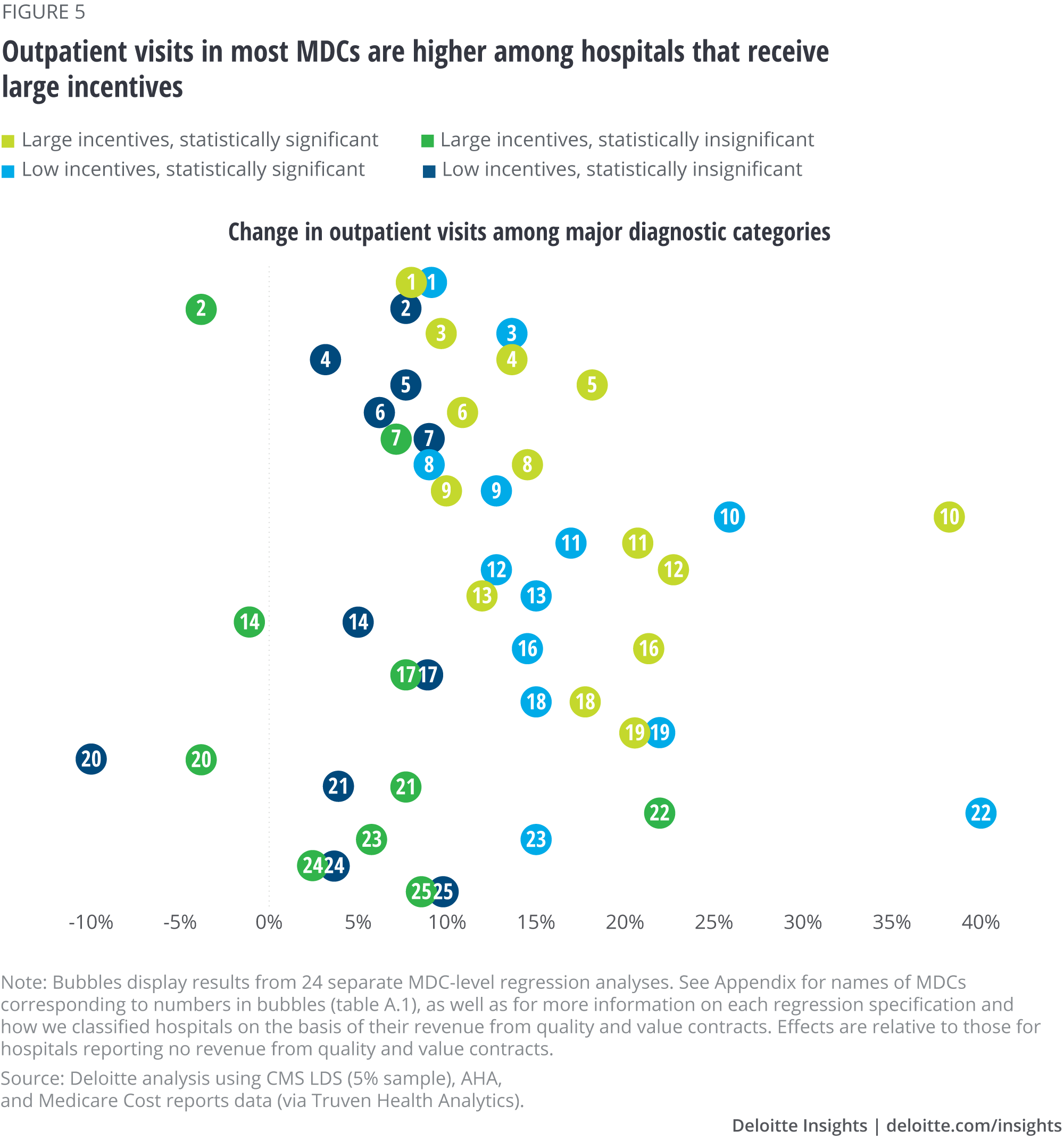
What might explain the relationship between incentives and outpatient book in the different therapeutic areas? Nosotros come across a stronger relationship between incentives and outpatient visits and revenue for therapeutic areas that have seen high physician-infirmary affiliation and technological change throughout the menses of our report. Amid physicians who bill Medicare, for example, 53 percent of cardiologists and 35 pct of orthopedists reported hospital or wellness system affiliation in 2014.19 Outpatient acquirement from diseases of the circulatory system20 was 18 percent higher among hospitals with large incentives (MDC 5 in figure 5). For diseases of the musculoskeletal system,21 outpatient revenue was 13 per centum college (MDC 8).
Examples of innovations in MDCs that are driving migration of handling to outpatient settings
Diseases and disorders of the musculoskeletal system. Light amplification by stimulated emission of radiation spine surgery is a minimally invasive procedure that no longer requires an inpatient stay. Endoscopy and live imaging are used to visualize the damaged disc, and the damaged tissue is removed using a precision laser. Since the surgical scar is modest, little or no postsurgery care is typically needed.22
Diseases and disorders of the circulatory organisation. Sure cardiology interventions—such as catheterization, percutaneous coronary intervention (PCI), and stent and percutaneous transluminal coronary angioplasties—are increasingly performed in outpatient settings.23 For instance, over 45 percentage of all PCI procedures shifted from the inpatient to the outpatient setting between 2004 and 2014.24 The change was largely driven past condom improvements stemming from clinical and technological innovations such as the use of radial access, less contrast material, bleeding risk assessments, meliorate anticoagulation options, and improved disposable products.
Diseases and disorders of the digestive system. A growing number of bariatric surgeries are performed on an outpatient ground. For instance, gastric balloons ingested by patients to achieve weight loss can now be removed endoscopically, without the demand for anesthesia or incision.25
Diseases and disorders of the ear, nose, pharynx, and mouth. Improvements in safety, combined with technological advancements such as "dropless" surgery, mean that virtually cataract surgeries can now be performed in outpatient settings.26
Diseases and disorders of the respiratory system. More than 70 percent of patients who undergo thoracoscopic surgery can be discharged on the day of surgery itself due to the utilise of new techniques and technologies such as brusk endoscopes with modest incisions and avant-garde robotic technological aids.27
Implications
Our original hypothesis was that we would find a more pronounced shift from inpatient to outpatient care among health systems with greater value and quality incentives. While we found college use of outpatient care, we did non find lower use of inpatient intendance than for other hospitals. I reason may be the very small proportion of hospitals with any blazon of incentive contracts at all, the relatively contempo experiences with these contracts, or the limited corporeality of risk these hospitals may be facing.
Nevertheless, it is interesting to detect that hospitals with incentives have greater outpatient services. Many hospitals are trying to increment their outpatient services both equally a defensive mechanism to react to new and more aggressive competitors and to diversify their revenues. Greater outpatient business concern may also position hospitals to do well under contracts that consider the whole spectrum of care in the hereafter and that reward closer medico-health organisation collaboration.
Going forward, hospitals and health systems, especially those that get a big portion of their acquirement from value contracts, will likely have to accost the need to motion handling from inpatient to outpatient settings. Is there a road map for this transition?
Health systems may want to consider their investments in both man and concrete capital. Expanding outpatient services may call for building partnerships with organizations that now accept the capacity (for example, ambulatory surgery centers, outpatient clinics, and retail centers) and human majuscule (physicians and other clinical staff) to support intendance in these settings, also as considerations around referral patterns, workflow, and operational improvements. Edifice physician relationships and networks through partnerships or affiliations can help increase chapters and attract patients. Chapters and capabilities tin can assist health systems succeed in both fee-for-service payment systems and value-payment arrangements.
Virtual care/engineering science can be a part of the outpatient strategy, allowing health systems to add capacity and generate referrals as well as provide a lower-cost setting for treatment.
Finally, technology tin can help wellness systems manage operations and patient care more than efficiently. For example, case management, supported past analytics, can help health systems work with patients to decide on which care setting is the almost effective, prophylactic, and efficient.
Appendix
The Deloitte Heart for Health Solutions performed regression analyses to written report the association between quality and value incentives and hospital inpatient and outpatient visits and acquirement. We used controls for factors that could influence this association, including hospital organizational characteristics (such as hospital size, urban/rural location, ownership type, service mix, teaching condition, and being part of a organization), case and payer mix, as well as local market weather.
The seemingly unrelated regressions model
Our main regression specification was a arrangement of 4 linear equations (one for each of the iv hospital service metrics) of the following class:
Hospital services metrics = f (quality and value incentive indicators, hospital organizational characteristics, case and payer mix, local market characteristics, and year indicators)
The variables are as follows:
- Infirmary services metrics. Outpatient and inpatient revenue and visits, in log course.
- Quality and value incentive indicators. Large incentives (hospitals with higher up the median share of acquirement coming from quality and value contracts); smaller incentives (hospitals with beneath the median share of revenue coming from quality and value contracts).
- Payer and case mix variables. Medicare and Medicaid shares in payer mix, an indicator for asymmetric share status, instance mix index, intensive intendance indicators, and nonacute share in total patient days.
- Hospital organizational characteristics. Indicator for the hospital being part of a arrangement, buying (indicators for regime and not-for-profit hospital ownership), and size (indicators for small and medium hospitals).
- Local marketplace conditions. Area wage mix index, disquisitional access indicator, urban location indicator, country indicators.
- Indicators for each year between 2012 and 2015.
In these models, the unit of observation is the hospital-yr cell. In the MDC analyses, the unit of observation is the hospital-MDC-year cell. Since we include country and twelvemonth indicators, the association between quality and value incentives and hospital service mix is estimated from changes in incentives in a given infirmary over time, as compared to other hospitals with similar characteristics in the same state. Nosotros use a seemingly unrelated regression estimation framework to account for the correlations betwixt our hospital service metrics, and we correct the standard errors for clustering on infirmary referral regions (HRRs). The adjusted R-squared in our estimations varied between 70 and 79 percent.
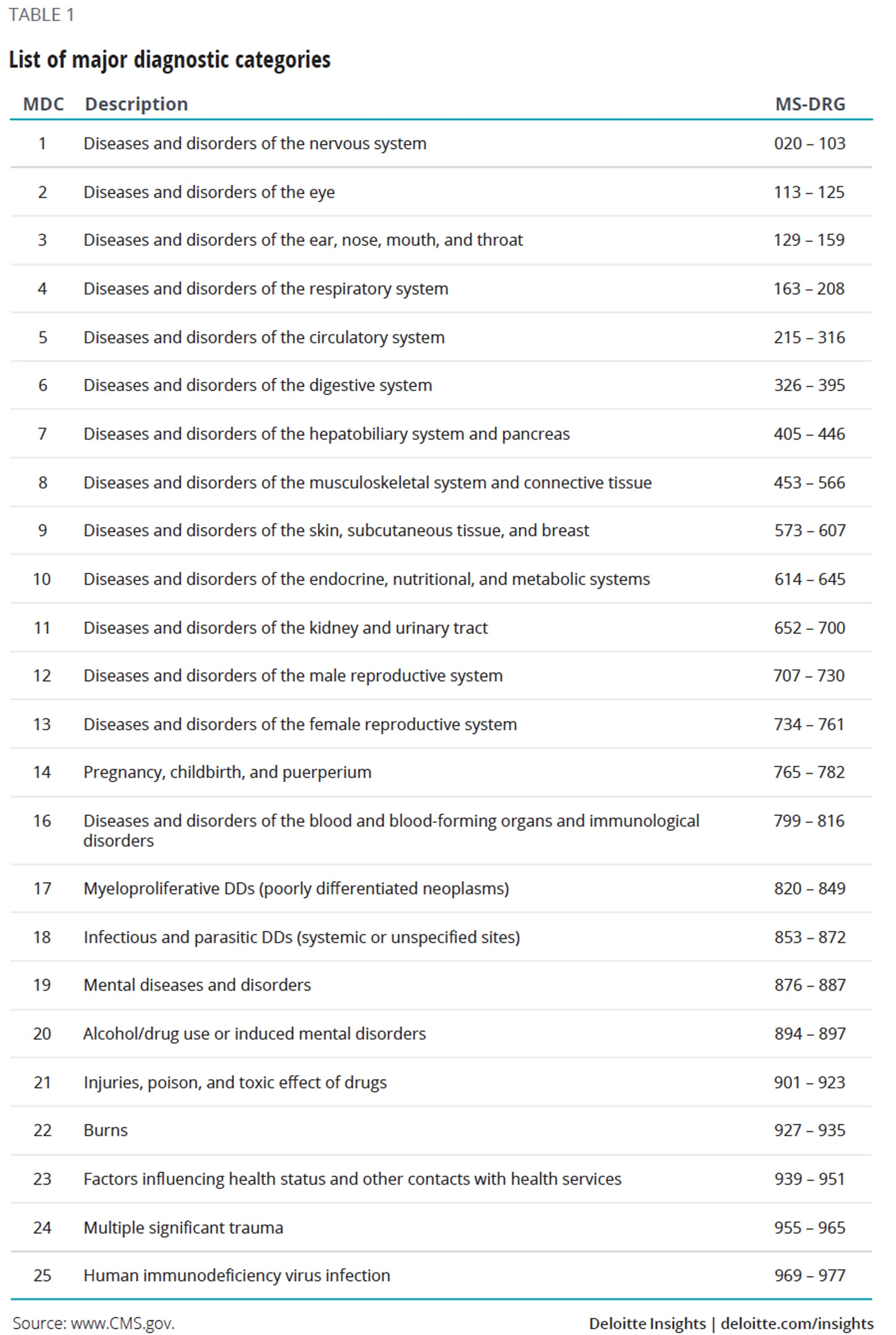
Major diagnostic categories (MDCs)
We mapped the ICD-9 and ICD-10 codes from the Medicare LDS claims information to their respective diagnosis-related groups (MS-DRGs), which were in plow mapped to their respective MDCs. MDCs were devised by physician panels to ensure DRGs are clinically coherent, since MDCs are mutually exclusive categorizations of all possible diagnosis codes. Each MDC corresponds to a single organ, system, or medical specialty. Public health departments28 use MDC coding in their inpatient discharge and emergency department modules.
In our information, information was not available for MDC 15 (newborns and neonates with atmospheric condition). The 24 other MDCs nosotros analyzed are listed beneath in table 1.
Source: https://www2.deloitte.com/us/en/insights/industry/health-care/outpatient-hospital-services-medicare-incentives-value-quality.html
Posted by: cainshead1975.blogspot.com


0 Response to "Which Of The Following Is The Primary Reason For The Growth In Outpatient Services?"
Post a Comment